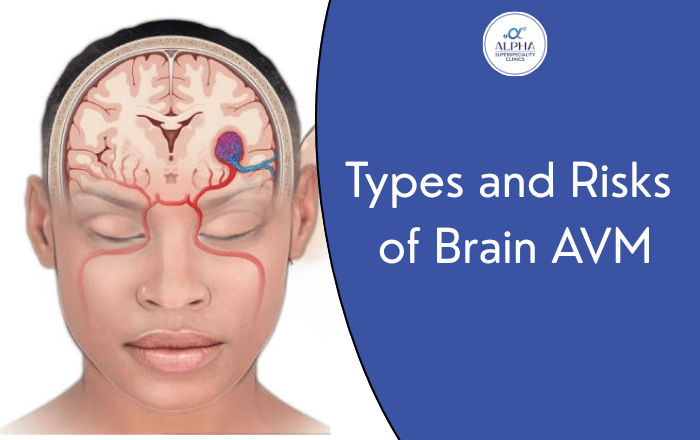
When you first hear the words “brain arteriovenous malformation” or “brain AVM,” it can feel overwhelming. You’re not alone in wondering what this means for you or your loved one. Think of a brain AVM as a tangle of blood vessels that formed incorrectly before birth – like a knot in a garden hose that changes how water flows through it.
Understanding the different types of brain AVM isn’t just medical jargon – it’s knowledge that can help you make informed decisions about treatment. Every brain AVM is unique, and doctors classify them based on three main factors: size, location, and specific risk factors. This classification helps determine the best approach for each person’s situation.
What Makes Each Brain AVM Different
Brain AVMs come in many shapes and sizes, and no two are exactly alike. Just like fingerprints, each one has distinct characteristics that affect how doctors approach treatment. The way medical professionals classify these brain AVM types helps them predict risks and plan the safest treatment path.
The most important thing to understand is that having a brain AVM doesn’t automatically mean you need immediate surgery. Many people live normal lives while managing their condition, and treatment decisions depend entirely on your specific type of AVM.
The Spetzler-Martin System: How Doctors Grade Brain AVMs
The Spetzler-Martin grading system is the standard way doctors classify brain AVM types. It’s like a report card that gives your AVM a grade from I to V, with Grade I being the simplest and Grade V being the most complex. This grading helps doctors understand the risks involved in different treatment approaches.
Size Matters: Small, Medium, and Large AVMs
- Small brain AVMs (less than 3 cm) are about the size of a walnut. These are often easier to treat and typically have better outcomes. Many small AVMs cause fewer symptoms and may be good candidates for surgery or radiosurgery.
- Medium AVMs (3-6 cm) are roughly the size of a lime. These require more careful planning, and doctors often consider multiple treatment options or a combination approach.
- Large brain AVMs (greater than 6 cm) are tennis ball-sized or larger. These complex cases often need special consideration, and sometimes careful monitoring is the safest choice rather than active treatment.
Location: Where Your AVM Lives in Your Brain
The location of your brain AVM plays a huge role in determining treatment options. Think of your brain as having “busy neighborhoods” and “quiet neighborhoods.”
Eloquent brain areas are the busy neighborhoods – places that control essential functions like speech, movement, memory, and vision. AVMs in these areas require extra caution during treatment because any damage could affect these critical functions.
Non-eloquent areas are the quieter neighborhoods where an AVM causes less risk to essential brain functions. AVMs in these locations often have more treatment options available.
Some specific high-risk locations include:
- The brainstem (controls breathing and heart rate)
- Areas controlling speech and language
- Motor regions that control movement
- Visual processing areas
Blood Flow Patterns: Superficial vs Deep Drainage
Brain AVMs also differ in how blood drains away from them. Superficial drainage means blood flows toward the surface of the brain, which is generally easier to manage. Deep drainage means blood flows toward the center of the brain, which can increase treatment complexity.
Understanding Your Risk Factors
Several factors influence how likely your brain AVM is to cause problems:
‣ Bleeding Risk
Most people want to know: “Will my AVM bleed?” The annual risk varies, but it’s generally around 2-3% per year for most unruptured AVMs. However, this risk changes based on your AVM’s characteristics and your personal health factors.
If your AVM has already bled once, the risk of future bleeding may be higher. This is why doctors take bleeding history very seriously when planning treatment.
‣ Age and Gender Considerations
Younger patients often have different treatment considerations than older patients. The brain’s ability to recover and adapt changes with age, which affects treatment decisions.
Women planning pregnancy may need special monitoring, as hormonal changes and the physical demands of pregnancy can sometimes affect AVM behavior.
‣ Lifestyle Factors
While you can’t change your AVM’s size or location, you can influence some risk factors:
- Keeping blood pressure well-controlled
- Avoiding activities that cause sudden blood pressure spikes
- Following your doctor’s medication recommendations
- Managing stress when possible
Treatment Options Based on AVM Type
The type of brain AVM you have largely determines your treatment options:
‣ Surgery
Grade I and II AVMs in non-eloquent areas are often good candidates for surgical removal. Surgery can provide a complete cure, eliminating future bleeding risk entirely.
‣ Radiosurgery
This treatment uses focused radiation beams to gradually close off the AVM. It works best for small to medium-sized AVMs in locations that are difficult to reach with traditional surgery.
‣ Embolization
This procedure uses tiny coils or glue to block blood flow through the AVM. It’s sometimes used alone or combined with other treatments.
‣ Careful Monitoring
For some high-grade AVMs or those in very risky locations, careful observation with regular check-ups may be the safest approach. This doesn’t mean “doing nothing” – it means actively managing your condition while avoiding treatment risks that might outweigh the benefits.
Living with Your Brain AVM Type
Knowing your brain AVM classification helps you understand what to expect. Many people with brain AVMs lead active, fulfilling lives. The key is working with your medical team to understand your specific situation and make informed decisions.
Regular follow-up appointments help monitor your AVM for any changes. Modern imaging techniques allow doctors to keep a close eye on your condition without invasive procedures.
Questions to Ask Your Doctor
Understanding your brain AVM type starts with asking the right questions:
- What grade is my AVM?
- Where exactly is it located in my brain?
- What are my treatment options?
- What would happen if we just monitor it?
- How often do I need follow-up scans?
Getting the Right Care in Pune
If you’re dealing with a brain AVM diagnosis, remember that you don’t have to navigate this journey alone. The complexity of brain AVM types and treatment options makes it important to work with someone who understands these conditions thoroughly.
Dr. Ninad Patil at Medicover Hospital in Bhosari, PCMC, specializes in treating all types of brain AVMs. With experience managing everything from simple Grade I AVMs to complex cases requiring careful consideration, Dr. Patil takes time to explain your specific situation and discuss all available options.
At Medicover Hospital, you’ll find a team that understands that behind every AVM classification is a person with hopes, concerns, and questions. Whether your AVM needs immediate attention or careful monitoring, having the right medical partner makes all the difference in your journey.
Take the Next Step
Don’t let questions about your brain AVM type go unanswered. Schedule a consultation with Dr. Ninad Patil at Medicover Hospital, Bhosari, PCMC, to discuss your specific situation. Understanding your AVM classification is the first step toward making informed decisions about your health.
Remember, every brain AVM is different, and what matters most is finding the right approach for your unique situation. With the right information and medical guidance, you can move forward with confidence, knowing you’re making the best decisions for your health and future.
Consult Dr. Ninad Patil, Brain Surgeon in Bhosari ,PCMC, for evaluation and treatment of brain AVMs and other neurological conditions.